Treatment of Pudendal Nerve Irritation, Groin and Perineal Pain
Pudendal nerve irritation, pudendal nerve entrapment, and perineal pain are all varying levels of symptoms related to pressure being created along the pathway of the pudendal nerve that creates very uncomfortable symptoms including:
-pain referring into the perineum, pelvic floor, groin, genitals (scrotum and penis in men/ labial & vagina pain, vaginismus and internally in women)
-pain into the genitals and perineum and around the back passage in men
-pain and tightness into the back of the hips
-posterior pelvic pain or pubic/ groin pain
-pelvic/perineal pain that is worse with sitting or when stressed, but that improves with standing or sitting on the toilet seat
-pain that is worse in tight clothing
The pudendal nerve originates from the lumbo-sacral plexus (L4-S4). It consists of both sensory fibers (80%) and motor fibers (20%). The pudendal nerve branches into 3 smaller nerves:
• Inferior rectal nerve: supplies the anal canal, peri-anal skin, rectum, and external anal sphincter.
• Perineal nerve: supplies the perineum, vagina, urethra, male scrotum, labia, transverse perineal muscle, and urethral sphincter.
• Dorsal nerve of the clitoris or penis: supplies skin of the clitoris/penis, bulbocavernosus, and ischiocavernosus muscles.
Pudendal nerve irritation, sometimes called pudendal neuralgia, may create changes in sensation in any or all areas the nerve supplies, and will tend to be associated with over-activity, or spasm of posterior pelvic floor muscles. This muscle over activity is thought to create narrowing of the pathway through which the nerve passes between sacrospinous and sacrotuberous ligaments (Alcocks canal), and/or between an interface created by ischiococcygeus, piriformis and obturator internus muscles.
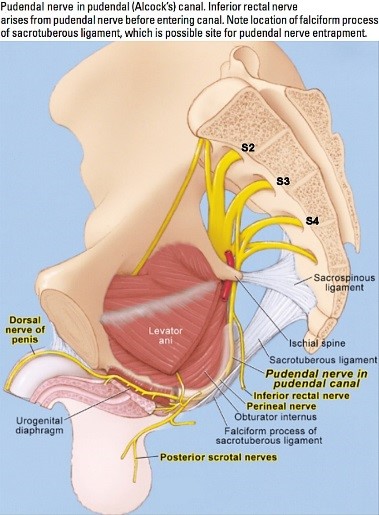
Figure 1: Pathway of the Pudendal nerve from the sacral plexus through Alcocks canal toward the genitals
Physiotherapy has proven to be a very successful treatment option for pudendal neuralgia, pudendal nerve irritation and pudendal nerve entrapment.
The key to understanding pudendal nerve irritation is to understand the anatomy of the posterior pelvis and how this part of the body is involved in our movements, stability, and daily life. Firstly, the pelvis is made up of 3 bones: the 2 innominates and the sacrum, with the coccyx being attached to the inferior pole of the sacrum. The pelvis is often considered to be the hub of the human skeleton because it connects between the spine and the legs, and has 35 muscles attaching onto it. The joints of the pelvis are also supported by some of the strongest ligaments in the body
Other nerves that supply to the groin/ scrotum and genitals include genito-femoral nerve and obturator nerve. These also need to be assessed in complex pelvic pain presentations
When you stand on 2 feet, 65% of your body weight is transferred from the base of your spine onto the top of the sacrum bone. This loading continues when you walk, sit, bend, run etc. In order to cope with the sorts of stresses we put across the joints in the lumbar spine and pelvis, the brain activates very specific muscles that support the joints. These muscles are often describes as our “core muscles”, but can also be visualized like a canister that encases our abdominal organs and supports the back and the pelvis (Hodges 20000).
Specifically the muscles of the core are:
Transversus abdominis: this muscle is the deepest muscle in the abdominal wall & it wraps around the lower abdomen from the belly button to the spine like a corset.
Lumbar multifidus: this is actually a series of small muscles that support each of the facet joints in the lumbar spine as well as tensioning the back part of the sacroiliac joint
Pubococcygeus: this is the front part of your pelvic floor, and it acts like the base of the canister, supporting under the organs and helping you to keep bladder and bowel control.
The way these core muscles work (or not) is important in the story of how Pudendal nerve irritation can develop. Research has shown that in a normal healthy body, the brain uses the core muscles to support your low back and pelvis whenever you shift your weight. That means, as you make the initial thought to move (for example from sitting to standing or standing to deciding to walk) the first reaction your brain will make is to turn on all these core muscles at about 5 to10% of their maximal force, without you thinking about it or being aware of it. The core muscle activity creates tension across joints of the low back, sacroiliac joints and pubic symphysis, and their continued activation maintains the support of these joints as your big muscles then turn on to create your movement. We rely on the feeling of stability we get from the core muscles working without us even thinking about it.
Poor postural habits, especially in sitting, stress, and back pain can all inhibit the way our core muscles should work. As our brain recognizes that the core muscles are not working, it starts looking for other options to try and hold us up. A common compensation strategy is for the brain to start gripping the deep buttock muscles, especially the ischiococcygeus and obturaot internus muscles. As these muscles start over working and tensioning constantly throughout the day, there is a chance that pressure is put onto the structures passing through Alcocks Canal, including the pudendal nerve.
The physiotherapists at Sydney Spine and Pelvis Centre are very aware of the different mechanisms that can lead to pudendal nerve irritation, and are actively involved in improving diagnosis and treatment of this painful condition. Our treatment plan includes assessing the pelvis and lumbar spine for articular or muscle dysfunctions, specific releases of the overactive muscles and tight ligaments, and teaching you how to turn the over active muscles off so that the nerve pressure can start to heal.
Please contact us on 02-97199114 if you would like to make an appointment for one of our team
An exercise to release Ischiococcygeus muscle and activate Pubococcygeus
- Imagine a triangle that has its tip at your pubic bone, and the back part of the triangle links your 2 sitz bones (ischeal tuberosities)
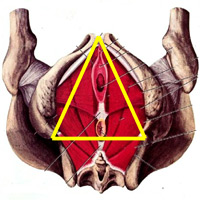
- The first step is to relax your bottom. Imagine your bottom is a block of chocolate, and you are lying on the beach on a hot summer's day. The sand is so hot it is making your chocolate melt. LET YOUR BOTTOM MELT OR RELAX. If the melting image doesn’t work, feel where your sitz bones are while lying down, and imagine these bones getting wider (or imagine the back part of your imagined triangle widening (don’t let your bottom squeeze and don’t let your sitz bones squeeze tight at all!!)
- Now keep the back part of your triangle wide, and imagine gently lifting the tip of the triangle (your pubic bone) up towards your belly button. Imagine a string connecting your pubic bone to your belly button that is gently tightening upwards. See if you can hold this without your bottom tightening, and breath.
- Which of the “images” helped to get your bottom relax? Keep practicing this when ever you feel your bottom tighten up and see if you can maintain this sense of relaxing the back of your traingle in sitting and standing
- GOOD LUCK!